|
Breast thermography is a diagnostic procedure that images the breasts to aid in the early detection of breast cancer.
The procedure is based on the principle that chemical and blood vessel activity in both pre-cancerous tissue and the area surrounding a developing breast cancer is almost always higher than in the normal breast. Since pre-cancerous and cancerous masses are highly metabolic tissues, they need an abundant supply of nutrients to maintain their growth. In order to do this they increase circulation to their cells by sending out chemicals to keep existing blood vessels open, recruit dormant vessels, and create new ones (neoangiogenesis). This process results in an increase in regional surface temperatures of the breast.
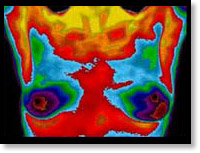 State-of-the-art breast thermography uses ultra-sensitive infrared cameras and sophisticated computers to detect, analyze, and produce high-resolution diagnostic images of these temperature and vascular changes. State-of-the-art breast thermography uses ultra-sensitive infrared cameras and sophisticated computers to detect, analyze, and produce high-resolution diagnostic images of these temperature and vascular changes.
The procedure is both comfortable and safe using no radiation or compression. By carefully examining changes in the temperature and blood vessels of the breasts, signs of possible cancer or pre-cancerous cell growth may be detected up to 10 years prior to being discovered using any other procedure. This provides for the earliest detection of cancer possible. Because of breast thermography's extreme sensitivity, these temperature variations and vascular changes may be among the earliest signs of breast cancer and/or a pre-cancerous state of the breast.(3,6,7,8,9)
Breast thermography has been researched for over 30 years, and over 800 peer-reviewed breast thermography studies exist in the index-medicus.
In this data base well over 250,000 women have been included as study participants. The numbers of participants in many studies are very large ranging from 37,000 to 118,000 women. Some of these studies have followed patients up to 12 years. Breast thermography has an average sensitivity and specificity of 90%.
Studies show that:
- An abnormal infrared image is also the single most important marker of high risk for developing breast cancer
- 8 times more significant than a first order family history of the disease(5).
- A persistent abnormal thermogram caries with it a 22x higher risk of future breast cancer.
- When added to a woman's regular breast health checkups, a 61% increased survival rate has been realized.
- Finally, when used as part of a multimodal approach (clinical examination + mammography + thermography) 95% of early stage cancers will be detected.
A positive infrared scan may indicate the presence of many different breast abnormalities such as mastitis, benign tumors, fibrocystic breast disease, cancer, and others.
Just as unique as a fingerprint, each patient has a particular infrared map of their breasts. Any modification of this infrared map on serial imaging (images taken over months to years) can constitute an early sign of an abnormality. In patients without cancer, the examination results are used to indicate the level of possible future cancer risk(4,5). Consequently, in the absence of other positive tests, an abnormal infrared image gives a woman an early warning. By maintaining close monitoring of her breast health with serial infrared imaging, self breast exams, clinical examinations, and other tests, a woman has a much better chance of detecting cancer at its earliest stage and preventing invasive tumor growth.
Breast thermography's ability to detect a pre-cancerous state of the breast, or signs of cancer at an extremely early stage, lies in its unique capability of monitoring the temperature variations and blood vessel alterations produced by the earliest changes in tissue physiology (function)(3,6,7,8,9).
However, thermography does not have the ability to pinpoint the location of a tumor. Consequently, breast thermography's role is in addition to mammography and physical examination, not in lieu of. Breast thermography does not replace mammography and mammography does not replace breast thermography, the tests complement each other. Since it has been determined that 1 in 8 women will get breast cancer, we must use every means possible to detect cancers when there is the greatest chance for survival (1). Proper use of breast self-exams, physician exams, thermography, and mammography together provide the earliest detection system available to date(3,7,8,9). If treated in the earliest stages, cure rates greater than 95% are possible(3,6).
The addition of breast thermography to the frontline of early breast cancer detection brings a great deal of good news for women.
References
- American Cancer Society – Breast Cancer Guidelines and Statistics, 1999
- I. Nyirjesy, M.D. et al; Clinical Evaluation, Mammography and Thermography in the Diagnosis of Breast Carcinoma. Thermology, 1986; 1: 170-173.
- M. Gautherie, Ph.D.; Thermobiological Assessment of Benign and Malignant Breast Diseases. Am. J. Obstet. Gynecol., 1983; V 147, No. 8: 861-869.
- C. Gros, M.D., M. Gautherie, Ph.D.; Breast Thermography and Cancer Risk Prediction. Cancer, 1980; V 45, No. 1: 51-56.
- P. Haehnel, M.D., M. Gautherie, Ph.D. et al; Long-Term Assessment of Breast Cancer Risk by Thermal Imaging. In: Biomedical Thermology, 1980; 279-301.
- P. Gamigami, M.D.; Atlas of Mammography: New Early Signs in Breast Cancer. Blackwell Science, 1996.
- J. Keyserlingk, M.D.; Time to Reassess the Value of Infrared Breast Imaging? Oncology News Int., 1997; V 6, No. 9.
- P.Ahlgren, M.D., E. Yu, M.D., J. Keyserlingk, M.D.; Is it Time to Reassess the Value of Infrared Breast Imaging? Primary Care & Cancer (NCI), 1998; V 18, No. 2.
- N. Belliveau, M.D., J. Keyserlingk, M.D. et al ; Infrared Imaging of the Breast: Initial Reappraisal Using High-Resolution Digital Technology in 100 Successive Cases of Stage I and II Breast Cancer. Breast Journal, 1998; V 4, No. 4
|
